Debridement of Fistula
Introduction
Debridement is the medical term used for removal of a patient’s dead, damaged, or infected tissue to improve the healing potential of the remaining healthy tissue. This removal may be achieved by surgical, mechanical, chemical, autolytic (self-digestion), or by maggot therapy (certain species of live maggots selectively eat only necrotic tissue). In oral hygiene and dentistry, debridement refers to the removal of plaque and calculus which have accumulated on the teeth.
In the process of debridement, the dead tissue called as eschar, debris or foreign material are removed from infected skin or wound. This promotes healing and also helps to control infection. There are several methods by which this can be accomplished. One method is excisional debridement in which the contaminated, infected or dead tissues are cut out or the affected structure or the organ part is removed surgically. Another method is non-excisional or mechanical debridement. The affected area is debrided by flooding it with an abundant amount of saline solution to wash away debris and other contaminants. This saline irrigation should not be confused with the surgical debridement of a wound, burn or other defect. Debridement is performed as a separate procedure when there is gross contamination which requires prolonged cleansing, when there is need to remove sizeable amounts of devitalized or contaminated tissues, or when debridement is carried out separately as a step to be followed in few days by primary closure. The reporting of debridement of the skin in the documentation reflects the type of debridement (excisional or nonexcisional), but does not necessarily need to document presence of healthy or viable tissues. Clear and concise documentation is critical for accurate reporting of excisional debridement. The documentation should be very specific regarding the type of debridement.
The goal of the treatment is to eradicate the fistula while preserving fecal continence at the same time
Some facts about fistula:
• Incidence of fistula is 8.6 per 100.000
• Nonspecific causes account for 90% cases of fistula
• Postoperative or traumatic cases are only 3%
• Fistulas arising from an anal fissure – 3%
• Fistulas arising from inflammatory bowel disease is also about 3%
• Tuberculosis – 1%
• It can also result rarely from anorectal malignancy, actinomycosis and lymphogranulomavenereum
• Average age of incidence is 38, men to women ratio is of 1.8 to 1
• Anorectal abscess may develop into fistula in some cases.
Clinical Manifestation:
• Non-healing anorectal abscess.
• Severe pain during defecation.
• Perianal itching.
• Associated symptoms (which depend on the underlying disease).
Imaging tests to be done for fistula diagnosis include:
1. Fistulogram
2. CT scan
3. MRI
4. Endosonography- accurate
Treatment:
The goal of the treatment is to eradicate the fistula while preserving fecal continence at the same time.
All fistula tracts with external openings within 3 cm of the anal verge and posterior to a line drawn through the ischial spines travel in a curvilinear fashion to the posterior midline. All tracts with external openings anterior to this line enter the anal canal in a radial fashion.
Treatment can be divided as:
1. Simple anal fistula
• Fistulotomy
• Track debridement and fibrin glue injection
2. Complex anal fistula
• Debridement and fibrin glue injection
• Endorectal advancement flap closure
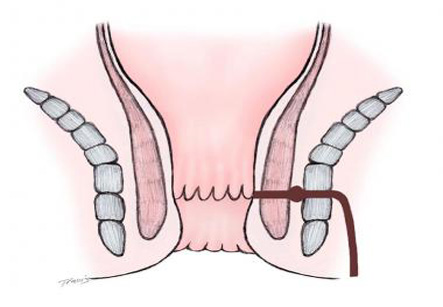
• Use of setonor staged fistulotomy
3. Crohn’s disease
• Asymptomatic Crohn’s disease need not be treated
• Simple, low Crohn’s fistula are treated by fistulotomy
• Complex Crohn’sfistula are treated with long-term draining setons.
• Complex Crohn’s fistula may also be treated with advancement flap closure if the rectal mucosa appears grossly normal